Topical Vitamin D
Vitamin D3 is manufactured from cholesterol, a sterol. It is made by the action of UVB sunlight as it strikes the cholesterol found in the epidermis and on bare skin.
Although initially a vitamin, it is converted by the liver to 25-OHD3 (calcidiol). This is then converted by the kidneys and other tissues to 1,25-OH2D3 (calcitriol), a potent steroid hormone. The skin has been found to have the ability to convert vitamin D3 into 1,25-OH2D3 (calcitriol).
Research published in late 2009, found a lack of vitamin D3 reduces the benefits of progesterone.
This is a short list below showing some of the actions of vitamin D3. All of which apply to progesterone. It...
- induces the anti-inflammatory Th2 response
- inhibits the Th1 inflammatory response
- suppresses inflammatory cytokines such as TNF-a, IL2 and IL6
- increases anti-inflammatory cytokines like IL-10
- inhibits mast cell secretions
- inhibits the oestrogen induced increase in dendritic spine density
- increases the expression of brain-derived neurotrophic factor (BDNF)
- positively affects neurologic functioning
- prevents neurodegeneration and enhance myelin repair
- positively affects motorneuron disease
- reduces damage in traumatic brain injury
- reduces hypertension
- regulates bone metabolism
- prevents lipid peroxidation
- is essential for pregnancy
- positively affects the skin and hair
- increases the concentrations of glutathione, the cells master antioxidant
- increases levels of superoxide dismutase, a powerful antioxidant
- inhibits mitosis, causing cell differentiation and apoptosis
- down-regulates the expression of glucocorticoids
- modulates fibroblast proliferation and collagen synthesis
Reduced levels of vitamin D3, progesterone too, are found in all the following diseases or disorders, and therefore constitutes an increased risk factor for...
- asthma and respiratory problems
- depression
- early ageing
- cancer
- epilepsy
- heart disease
- migraines/headaches
- polycystic ovaries
- miscarriage
- fibroids
- peripheral neuropathy (nerve pain)
- myopathy
- autoimmune diseases, such as MS, lupus, Sjogren's syndrome, arthritis etc
- SAD (seasonal affective disorder)
- Alzheimer's disease
There seems some uncertainty about what constitutes an adequate level. The NHS in the UK stating 20ng/ml (50nmol/L) is adequate. The FDA have set their adequate level at 30ng/ml (75nmol/L). Whereas vitamin D3 specialists are arguing for a minimum of 50ng/ml (125nmol/L), some suggesting a range of 70-100ng/ml (175-250nmol/L).
Studies in rural communities have found levels ranging from 23.2ng/ml (58nmol/L) to 68.4ng/ml (171nmol/L), giving a median of 46ng/ml (115nmol/L).
Two interesting findings came out of the studies. One that vitamin D levels do not drop with age, and in fact increase. One 65 year old having a level of 70ng/ml (175nmol/L). And that pregnant women had high levels. One pregnant woman in fact had a level of 105ng/ml (262.5nmol/L), 5ng/ml higher than a level many regard as toxic!
The people most affected by a lack of vitamin D are those with the darkest skin living in higher latitudes. Skin type is critical to vitamin D3 production, the darker the skin the more time in the sun is required to produce it.
A 2010 study published in America found 90% of the darker skinned people, and three quarters of the white population had levels below 30ng/ml.
Vitamin D is fundamental to cellular health, the vitamin D receptor is found in every cell. It directly or indirectly regulates up to 2,000 genes.
The outermost layer of skin is called the epidermis. It comprises 90-95% keratinocytes. The function of these specialised cells is to produce keratin, the tough protective layer covering the outer surface. This prevents bacteria, fungi, parasites and viruses from entering the skin. They also protect from UV radiation and water loss. Another function is to produce defensive substances which kill the pathogens.
Keratinocytes in the skin have ample vitamin D receptors, and are capable of converting vitamin D3 into 1,25 (OH)2D3 or calcitriol, the active metabolite. Calcitriol in turn regulates epidermal proliferation and differentiation. Topical application has been found effective against psoriasis, a hyper-proliferative state of keratinocytes. Psoriatic patients have low vitamin D levels. Keratinocytes also have ample progesterone receptor sites.
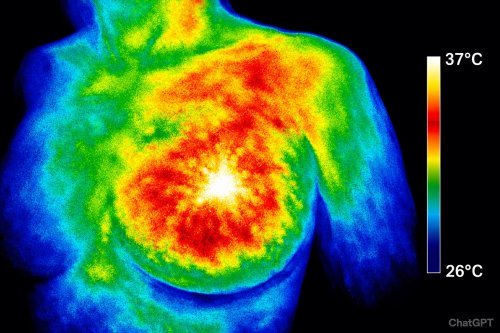
Although the skin makes vitamin D3 from UVB rays, it also suffers from UVB and UVA damage. This can cause a significant increase in free radicals. In particular UV radiation causes a rapid and significant increase in hydrogen peroxide levels. Free radicals damage DNA, cause inflammation, death of skin cells, skin ageing and skin cancer. Vitamin D has a photo protective effect, reversing the above effects. It's a powerful anti-inflammatory and antioxidant too, as is progesterone.
UV light causes photo ageing by inducing matrix metalloproteinases (MMPs). These enzymes break down skin connective tissue, causing a pathological reaction such as inflammation and tissue degeneration when in excess. Excess oestrogen also stimulates MMPs, it accelerates the ageing of collagen too. Vitamin D and progesterone are natural inhibitors of MMPs.
1,25-OH2D3 (calcitriol) stimulates the production of cathelicidin and -defensin in all cells, including kerotinacytes. These are antimicrobial substances that protect the skin against bacterial attack. One could call them the body's own antibiotics. Cathelicidin also promotes wound healing, tissue repair and heals inflammation.
One study says...
"Humans with deficient cathelicidin production... are prone to infections of epithelial surfaces such as the skin and mucosal membranes. Therefore, anti-microbial peptides such as cathelicidin constitute an integral part of the innate immune response to a variety of infections especially at barrier sites."
Sebocytes have been identified as 1,25(OH)2D3-responsive target cells. Sebocytes are highly specialised, sebum-producing epithelial cells. Sebum forms an integral part of the epidermal barrier and the immune system of the skin. Lauric acid, an extract of coconut oil, dramatically enhances the expression of human beta-defensin in skin sebocytes.
Sebum synthesis is regulated by hormones, in particular the androgens. Excess androgen production leads to excessive sebum production, as seen in acne. Progesterone inhibits the secretion of androgens by increasing sex hormone binding globulin. It also inhibits 5-alpha reductase, the enzyme that converts testosterone into DHT, implicated in acne.
Inflammatory skin diseases can benefit from topical applications of vitamin D3 and progesterone, together with lauric acid. This has bactericidal properties and acts as a natural antibiotic against Propionibacterium acnes which causes inflammatory acne.
As vitamin D3 is made naturally in the skin, and is then transported from the epidermal layer down into the blood vessels, topically applied vitamin D3 is also transported into the blood stream. It does raise blood levels of vitamin D.
Because keratinocytes have the ability to convert vitamin D3 into calcitriol, supplying additional vitamin D3 to the skin should increase the calcitriol content without harm. Calcitriol is a potent hormone, people given it to take can develop resistance.
One 2012 study found people with low levels of vitamin D had lower average skin moisture. They state further that...
"Topical supplementation with cholecalciferol significantly increased measurements of skin moisturization and resulted in improvements in subjective clinical grading of dry skin. Taken together our finding suggest a relationship between serum vitamin D(3) (25(OH)D) levels and hydration of the stratum corneum and further demonstrate the skin moisture benefit from topical application of vitamin D(3)."
Basal cell carcinomas (BCCs) are the most common of all human cancers, affecting 1 million people in America. Squamous cell carcinoma (SCC), another skin cancer, is found in about 700,000 people. Hedgehog (HH) signalling underlies several human tumours, including basal cell carcinoma. Several studies are currently testing synthetic inhibitors of HH signalling against at least 8 human cancers.
Sebocyte formation is controlled by various molecular pathways, one of which is also the Hedgehog pathway.
Topical vitamin D3 blocks both proliferation and HH signalling in BCC cells in vitro and in vivo.
The study found that...
"These results are specific for vitamin D3, because the precursor 7-dehydrocholesterol and the downstream products 25-hydroxy vitamin D3 [25(OH)D] and 1,25-dihydroxy vitamin D3 [1,25(OH)2D] are considerably less effective in reducing ...cellular proliferation."
Merkel cell carcinoma (MCC) is a rare, but aggressive skin cancer, it's incidence is rapidly increasing. Could this be due to the fact most people have low vitamin D levels, because of avoiding the sun? MCC appears to be caused by Merkel cell polyomavirus and is associated with low vitamin D levels. No study on the topical use of vitamin D3 has been done. But judging by the results from the BCC study, topical vitamin D3 might be protective.
In addition to mutated HH signalling, human BCCs also have mutations in gene p53. This is commonly called the 'guardian of the genome'. Damage to p53 is caused by UV rays. A loss of this greatly accelerates BCC carcinogenesis. Interestingly, p53 controls the tanning process, a loss of p53 or mutations of it would lead to DNA damage and burning rather than tanning, and thence to cancer. Both vitamin D and progesterone activate p53.
One study on Merkel cell carcinoma found "The observed overexpression of p53 suggests that the development of this tumor type may be related to chronic ultraviolet damage"
Vitiligo is another skin condition where low levels of vitamin D have been found. Topical analogues of vitamin D have found limited success. Narrow band UVB light has had a measure of success. Adding topical calcipotriol, a vitamin D analogue, showed no advantage. Apart from the two studies quoted above on skin moisturising and BCC, little cognisance is taken of topical vitamin D3.
A topical vitamin D skin cream containing vitamin D3 and lauric acid, and not the usual 1,25-OH2D3 (calcitriol) would appear a safe and effective means of helping the skin heal and prevent skin cancer.
Vitamin D3 is essential for health, have a blood test done to check the level. The test should only be done for 25-hydroxyvitamin D3, also called calcidiol.
Blood levels should be 70-100ng/ml or 175-250nmol/L and not the 30ng/ml or 75nmol/L most labs and doctors regard as adequate.
The minimum daily dose should be at least 5000iu's per day, although the latest research indicates optimal dosage at 10,000iu's per day, see here.
For more information on vitamin D see these websites...
- Vitamin D Council
GrassrootsHealth
Birmingham Hospital
Michael F. Holick
Factors Influencing Vitamin D Status
Natural sunscreens
For more detailed information on topical vitamin D and reference papers.
For more information on progesterone see...
 Memory is the brain’s ability to store and recall information. When this system fails, we experience memory loss, which ranges from mild forgetfulness to severe cognitive impairment such as dementia o…
Memory is the brain’s ability to store and recall information. When this system fails, we experience memory loss, which ranges from mild forgetfulness to severe cognitive impairment such as dementia o…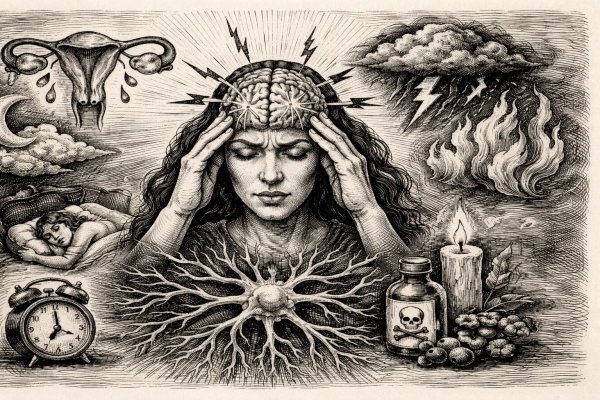 Migraines aren’t just intense headaches — they’re a systemic neurological crisis that disrupts your senses, drains your energy, and derails your life. What most people don’t realize is that women are…
Migraines aren’t just intense headaches — they’re a systemic neurological crisis that disrupts your senses, drains your energy, and derails your life. What most people don’t realize is that women are…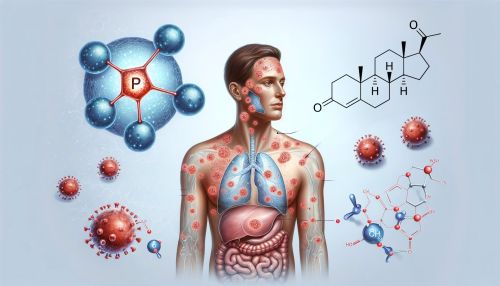 Psoriasis is commonly seen as a skin problem — red, scaly patches that itch and flare without warning — but research shows the real driver may be hormonal imbalance deep inside the body, especially lo…
Psoriasis is commonly seen as a skin problem — red, scaly patches that itch and flare without warning — but research shows the real driver may be hormonal imbalance deep inside the body, especially lo…