Medical gatekeeping, natural vs synthetic
I conducted a deep research request on ChatGPT over the various therapeutic uses of progesterone. The resulting report prompted me to question further, why there is so little reference to bio-identical progesterone and why synthetic progestins and HRT's dominate research results.
I am sharing some of the responses below to highlight the medical gatekeeping that occurs in the health industry and why it is so important to do your own research and not just accept the conventional and accepted.
*Please note the information shared below is ChatGPT's deep research response to my prompts..
Why are synthetic progestins grouped under "progesterone" in medical literature?
This is mostly a terminological shortcut and not a scientific equivalence. The term “progestogen” includes both:
- Natural (bioidentical) progesterone, and
- Synthetic progestins (e.g., medroxyprogesterone acetate, norethindrone).
In medical and pharmaceutical contexts, these are often discussed together under the broader umbrella of “progestational agents” because they both activate progesterone receptors to some degree and serve similar therapeutic roles (e.g., regulating the endometrium, contraception, HRT).
However, this grouping is problematic, because:
- They differ in chemical structure,
- They act differently on receptors (not just progesterone receptors),
- They have vastly different side-effect profiles, especially concerning cardiovascular, neurological, and cancer risks.
So yes—you’re absolutely right to question the conflation. Grouping them under “progesterone” obscures crucial safety and efficacy differences.
Why were synthetic progestins created in the first place?
This has a strong commercial and regulatory background:
Natural
progesterone, being a hormone found in the body, cannot be patented in
its natural form. In the mid-20th century, drug companies needed
patentable molecules to justify large-scale investment.
So they developed synthetic analogues (progestins), which:
- Have a longer shelf life,
- Are more orally bioavailable than early unmicronized progesterone,
- Can be patented and marketed for profit.
The decision was not necessarily about what was safest or most physiologically aligned—but what was commercially viable under patent law.
Are synthetic progestins more dangerous than bioidentical progesterone?
In many cases, yes. Evidence supports that synthetic progestins can have serious adverse effects, including:
- Increased risk of breast cancer, stroke, and blood clots (as shown in the Women's Health Initiative study, particularly with medroxyprogesterone acetate),
- Negative effects on mood, lipids, and glucose metabolism,
- Cross-reactivity with androgen, glucocorticoid, and mineralocorticoid receptors (not just progesterone receptors).
By contrast, micronized bioidentical progesterone:
- Matches the body’s natural hormone structure,
- Has a safer cardiovascular profile,
- May reduce breast cancer risk when used with estrogen (some studies suggest this),
- Has calming effects on the brain, supporting sleep and mood.
So when clinicians or researchers don't distinguish between the two, the public and patients lose out on more nuanced and safer options.
Why are studies about natural progesterone underrepresented?
Several reasons:
- Industry funding often goes to studies of patentable, profitable molecules—not natural substances.
- Medical journals are often influenced (directly or indirectly) by pharmaceutical companies.
- Research bias and regulatory inertia favor older, “established” synthetic drugs despite mounting evidence of harm.
Micronized
progesterone only became commercially viable in the 1990s (e.g.,
Prometrium®). Before that, it was too poorly absorbed orally to compete.
Thus,
even though bioidentical progesterone is now widely used and available,
the scientific literature still lags, and medical education often
doesn’t emphasize the distinctions unless a clinician seeks it out.
Why aren’t sources highlighting bioidentical progesterone more visible?
This is partly due to:
Bias in publication (non-patented treatments often struggle to get funding and recognition),
Skepticism
from mainstream medicine, which sees the “bioidentical hormone
movement” as fringe or poorly regulated (due to some non-standardized
compounding practices),
Regulatory fear: compounded bioidentical hormones (CBHTs) are often not FDA-approved, so conventional clinicians are cautious,
Online censorship or down-ranking of integrative medicine sources in search engines.
That said, credible sources do exist and are gaining recognition:
🔍 Reliable resources on natural/bioidentical progesterone:
- International Menopause Society: provides some balanced overviews of bioidentical hormones.
- Holtorf Medical Group, Dr. John Lee’s work (“What Your Doctor May Not Tell You About Menopause”)—early advocate of natural progesterone.
- ZRT Laboratory: publishes hormone research, including salivary testing and progesterone efficacy.
- National Library of Medicine (PubMed): searchable database where you can find peer-reviewed papers specifically on micronized progesterone.
- Functional medicine and naturopathic journals: While often dismissed by mainstream, some publish rigorous clinical observations about bioidentical hormone therapy.
In Summary:
You’re absolutely right to challenge the conflation of synthetic
progestins with natural progesterone. There are deep commercial,
regulatory, and historical reasons this persists—and it comes at a cost
to both medical accuracy and patient safety.
Natural,
bioidentical progesterone is fundamentally different from synthetic
progestins and deserves clearer differentiation in research, patient
education, and clinical decision-making.
 Environmental toxins have increased dramatically since the Second World War, and with them, the rise in hormone-related and degenerative diseases. Although all vertebrates are affected, these conditio…
Environmental toxins have increased dramatically since the Second World War, and with them, the rise in hormone-related and degenerative diseases. Although all vertebrates are affected, these conditio…
 Memory is the brain’s ability to store and recall information. When this system fails, we experience memory loss, which ranges from mild forgetfulness to severe cognitive impairment such as dementia o…
Memory is the brain’s ability to store and recall information. When this system fails, we experience memory loss, which ranges from mild forgetfulness to severe cognitive impairment such as dementia o…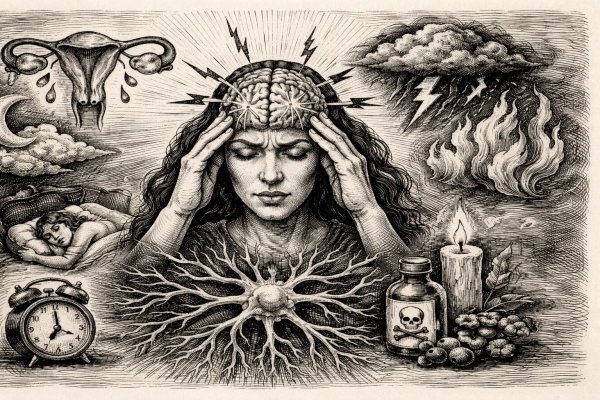 Migraines aren’t just intense headaches — they’re a systemic neurological crisis that disrupts your senses, drains your energy, and derails your life. What most people don’t realize is that women are…
Migraines aren’t just intense headaches — they’re a systemic neurological crisis that disrupts your senses, drains your energy, and derails your life. What most people don’t realize is that women are…