Body Acne reaction to progesterone therapy
by Billie Jo
(USA)
Hi Wray,
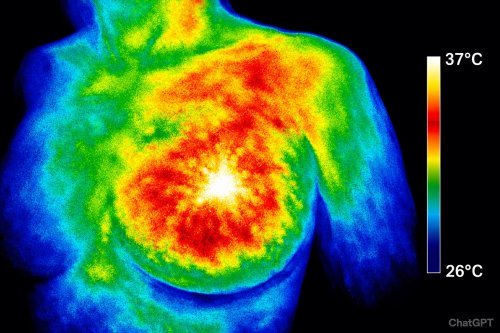
I am 37 years old. I had a history of endometriosis my whole life. I saw a specialist this year who also told me I had PCOS, not due to cysts necessarily but due to insulin resistance. That diagnosis was based on lab results which showed insulin resistance as well as reactive hypoglycemia. During my workup prior to surgery (he is a specialist in excising endometriosis), I noted I was having hot flashes, night sweats, lack of focus, fits of rage. All of this seemed to point him to premature ovarian failure. He started me on an estradiol patch (minivelle) while I had some tests done to help him confirm his suspicions. When the tests came back, I was surprised he had not tested my estradiol levels at all. He did test for the LH which was normal. He also tested serum testosterone and serum levels of DHEA-S, both of which were high but the DHEA-S was through the roof so to speak (360’s). Even after tests came back and I reported no relief of symptoms on the patch, he still insisted I needed the extra estrogen. He is also a reproductive endocrinologist, so against my better judgement I forced myself to trust in his methodology. He assured me it was estrogen that I needed and I just needed more. He stated the patch didn’t work for everyone and that it was most likely an absorption issue. So he prescribed me with an estradiol tablet to be vaginally inserted. I began that therapy and after 1 month saw no improvement, only weight gain and added headaches. Then he suggested we up the dosage, so we did. Instead of breaking the tablet in half and using that once a day, I would break it in half and use that twice a day. Shortly after beginning this increase, I awoke one morning to blood covering a large portion of the white in my right eye. I immediately went to my eye doctor and was diagnosed with subconjunctival hemorrhage of the right eye. I stopped the estrogen therapy. This event really freaked me out. It took about a week for the blood in my eye to dissipate. By then, it was time for my pre-op appointment with my doc. I told him I had stopped the estrogen therapy and why. He assured me that the extra estrogen didn’t cause my eye situation. He reiterated my need for extra estrogen and that we just needed to increase the dosage again. At the appointment, I also discovered his plan was to remove not only my uterus and cervix (due to severe adenomyosis) but also my tubes and ovaries at surgery. Removal of the tubes was all that we had discussed but never the ovaries. I was shocked to say the least. My thoughts were, if it’s estrogen he says I need, why the heck are we taking the ovaries out? (somethings better than nothing was my thinking). He told me that it was up to me, but that he recommended taking them and that I could decide even up to just before surgery on that. I needed to know what my levels were at the very least so I went to a lab and had them tested. Unfortunately the results didn’t make it back in time before my surgery. However, I was confident that I should hang on to my ovaries if they were not diseased. So that’s what I did.
My surgery was on 5/1/18. It was a total hysterectomy (uterus & cervix), salpingectomy and excision of stage 2 endometriosis. I felt great after! The pain is gone. And in terms of the pain I have experienced since I was 11, this surgery was the first step to me getting my life back.
Now we come to the second step. So I never started the estrogen therapy back up, even though my doctor wanted me too. It just never felt right. And, I thought I was actually done with all my hormone problems. I know that endometriosis creates its own estrogen and I had figured that its removal had corrected my issues. The night sweats went away and the hot flashes went away. But then, after about 3 weeks, I started to feel just really hormonal, PMS style symptoms but to the degree that the fits of rage scared me. I had hoped these were gone with the pain. But, they were back and with a vengeance. I have 3 kids and, this symptom was problematic in a number of ways and was just simply one I could not afford to just let go unchecked. So I began to read more about hormones.
In my research, I came across your page that suggested I should try progesterone. I did a saliva test through ZRT labs which results came back on 6/15/18 and are as follows:
estradiol — 1.9
progesterone — 62
ratio: Pg/E2 — 33
Testosterone — 53
DHEAS — 36.5
(as well as all day cortisol levels which came back normal)
During that time, I had already ordered your 3 pack of airless pump bottles of Natpro and had begun using them. I received the bottles June 8th and began the therapy that day.
After reading about the side effects of using too little, I decided I would start out with 300mg per day split into 2 dosages (morning and evening) of 150mg which was 3 pumps. I didn’t notice any positive changes. I had developed a few pimples here and there and I had noticed a problematic varicose vein in my right leg becoming worse. I had hoped to see some of the water retention dissipate, maybe an increase in energy levels, and a possible downward trend to the rage. Nevertheless, I continued to proceed with that same dosage. I have gone through 1 complete bottle and am on the second bottle.
This brings me to my current situation. I began to notice bumps (acne really) developing on my abdomen. I had rotated where I applied the cream so I new that wasn’t the problem. I read a few different threads on your page and determined it was likely that this was the estrogen fighting back, so I increased the dosage by adding another 2 pumps (100mg) mid day, which brought my daily dosage to 400mg. The acne got far worse after about 3 days of that. My entire back was/is covered, have it on my abdomen and breasts as well as it developed on my arms and legs. It is itchy and, well, gross looking to say the least. This is day 4 of the full blown reaction. Day 1 I continued as normal; Day2 I only did 1 treatment of 100mg; Day 3 (yesterday) was my first day with no progesterone and the bumps began to become scaly and are drying out. Today I do not plan on applying the cream either.
I want to trust the process but this reaction was very concerning. I also became very lethargic and just feeling very uneasy on Day 2 when the reaction was at its peak.
What are your thoughts?
Comments for Body Acne reaction to progesterone therapy
|
||
|
||
 Memory is the brain’s ability to store and recall information. When this system fails, we experience memory loss, which ranges from mild forgetfulness to severe cognitive impairment such as dementia o…
Memory is the brain’s ability to store and recall information. When this system fails, we experience memory loss, which ranges from mild forgetfulness to severe cognitive impairment such as dementia o…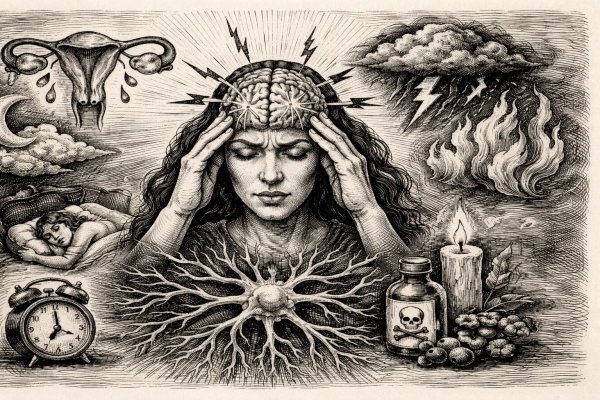 Migraines aren’t just intense headaches — they’re a systemic neurological crisis that disrupts your senses, drains your energy, and derails your life. What most people don’t realize is that women are…
Migraines aren’t just intense headaches — they’re a systemic neurological crisis that disrupts your senses, drains your energy, and derails your life. What most people don’t realize is that women are…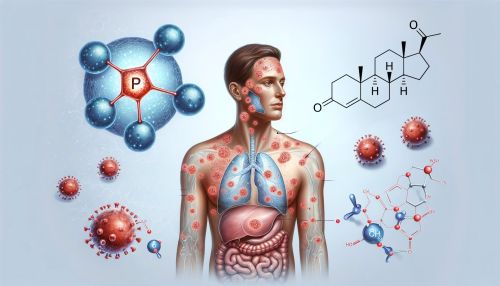 Psoriasis is commonly seen as a skin problem — red, scaly patches that itch and flare without warning — but research shows the real driver may be hormonal imbalance deep inside the body, especially lo…
Psoriasis is commonly seen as a skin problem — red, scaly patches that itch and flare without warning — but research shows the real driver may be hormonal imbalance deep inside the body, especially lo…