Progesterone metabolism and transdermal supplementation
Progesterone Metabolism in the Body
When your body makes progesterone (endogenous) (in the ovaries, adrenal glands, or even in smaller amounts from peripheral tissues), it circulates through the bloodstream mostly bound to proteins such as albumin and corticosteroid-binding globulin. Only a small portion of progesterone is ‘free’, but this is the part that can bind to progesterone receptors in tissues.
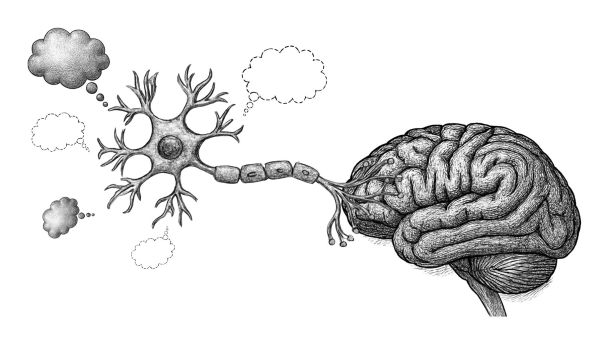
Progesterone exerts its effects by binding to two main receptor types, called PR-A and PR-B, which are found in many tissues: the uterus, brain, breasts, skin, bone, and cardiovascular system. Beyond this genomic signaling, progesterone also has non-genomic actions - fast-acting effects on cell membranes and neurotransmitter systems.
Once progesterone has circulated and interacted with target tissues, it is metabolised. Most metabolism occurs in the liver, although some happens locally in tissues as well. The main pathways include:
• Conversion by 5α-reductase and 5β-reductase into di-hydroprogesterone derivatives.
• Further conversion into allopregnanolone and pregnanolone, potent neuroactive steroids that modulate the GABA-A receptor, producing calming, anxiolytic, and sleep-enhancing effects.
• Hydroxylation at various positions (such as C20 and C21).
• Conjugation with glucuronic acid or sulfate, making metabolites water-soluble for excretion.
Finally, progesterone metabolites are eliminated primarily through the urine as pregnanediol glucuronide or through bile into the faeces.
Progesterone is not ‘wasted’ when metabolised. Its metabolites are biologically active, particularly allopregnanolone, which many researchers now consider a critical factor in progesterone’s mood-stabilizing and neuroprotective actions.
What happens when you apply progesterone transdermally?
When natural progesterone is applied to the skin in the form of a cream or gel, a different route of delivery comes into play. Instead of entering the digestive system and being metabolised immediately by the liver (the so-called ‘first-pass effect’), transdermal progesterone is absorbed through the skin and enters the capillaries of the dermis. From there, it binds to proteins in the blood and is delivered to tissues.
Here is an overview:
1. Absorption through the skin
Progesterone is lipophilic, meaning it dissolves in fat. This allows it to move through the stratum corneum, the outermost layer of skin. Absorption occurs not just by diffusion through skin layers, but also via the hair follicles and sebaceous glands, which provide a direct pathway inward.
2. Bypassing the liver
Unlike oral progesterone, which is rapidly broken down in the liver, transdermal progesterone avoids this ‘first-pass metabolism’. This means more intact hormone can reach tissues before being metabolised.
3. Distribution to tissues:
Once in circulation, progesterone delivered via a cream behaves the same as endogenous progesterone. It binds to receptors in the uterus, brain, breast, bone, skin, and other tissues. Importantly, the skin itself expresses progesterone receptors — so some benefits occur locally at the site of application before the hormone even reaches the bloodstream.
4. Metabolism and excretion
After exerting its effects, transdermally delivered progesterone undergoes the same metabolic pathways as natural progesterone, eventually being transformed into neuroactive and inactive metabolites, conjugated, and excreted in urine and bile.
Clinical studies show that topical progesterone raises levels in capillary blood and saliva, even if serum blood levels do not always reflect the increase. This is why conventional lab testing sometimes underestimates the effectiveness of creams — serum reflects only one compartment, whereas tissue and saliva levels often tell a different story.
The Role of 5α-Reductase in the Skin: Clearing Up the Confusion
The skin, particularly sebaceous glands and hair follicles, expresses 5α-reductase. This enzyme is best known for converting testosterone into DHT. It can also convert progesterone into 5α-dihydroprogesterone, a precursor of allopregnanolone.
But here’s the important point:
•While some progesterone is metabolized locally in the skin, research shows that a significant fraction still passes through intact, entering systemic circulation.
*In fact, measurable rises in progesterone are found in tissues, saliva, and capillary blood after topical application.
*Most conversion into neuroactive metabolites like allopregnanolone happens after absorption, in the liver and nervous system — not primarily in the skin.
The skin is both an absorptive surface and a living tissue that contributes to local hormone activity.
Transdermal vs oral progesterone: key differences
Understanding the differences between oral and transdermal delivery can help explain why creams are often preferred for ongoing therapy.
Oral Micronised Progesterone
- Undergoes extensive first-pass liver metabolism.
- Produces higher levels of allopregnanolone, which explains its sedative effect (often used at night for sleep).
- Serum levels rise, but much of the progesterone is metabolised before reaching peripheral tissues.
Transdermal Progesterone
- Bypasses the liver initially, delivering intact hormone directly to tissues.
- Does not cause the same degree of the sedative effect, since less immediate conversion to allopregnanolone occurs in the liver.
- Provides steady, natural support to tissues and receptors throughout the body.
Both routes have their place, but for many women, transdermal bio-identical progesterone provides effective symptom relief without the drawbacks of oral administration.
See our page on progesterone application methods for more details.
Progesterone is not just a ‘fertility hormone’. It has profound effects throughout the body: calming the nervous system, protecting the brain, counterbalancing estrogen, supporting bone, skin, and cardiovascular health.
Understanding how progesterone is metabolised, and how supplementation works, helps clear up the myths that often discourage women from using natural progesterone.
The truth is simple:
• Progesterone metabolism is a natural process that creates powerful metabolites with their own beneficial effects.
• Transdermal supplementation does not 'waste' progesterone in the skin; rather, it delivers meaningful amounts to circulation and tissues.
• Bio-identical progesterone, delivered through the skin, remains an effective, safe, and natural way to restore balance.
See our page Effects of Progesterone for more information.
References
1.Stanczyk FZ, Paulson RJ, Roy S. Percutaneous administration of progesterone: blood levels and endometrial protection. Menopause. 2005 Mar;12(2):232-7. PMID: 15772572.
2. Carey BJ, Carey AH, Patel S, Carter G, Studd JW. A study to evaluate serum and urinary hormone levels following short- and long-term administration of two regimens of progesterone cream in postmenopausal women. BJOG. 2000;107(6):722–726. [PMID: 10847227]
3. Vashisht A, Wadsworth F, Carey A, Carey B, Studd J. A study to look at hormonal absorption of progesterone cream used in conjunction with transdermal estrogen. Gynecol Endocrinol. 2005 Aug;21(2):101-5. doi: 10.1080/09513590500128583. PMID: 16109596.
4. Zargar-Shoshtari S, Wahhabaghei H, Mehrsai A, Wen J, Alany R. Transdermal delivery of bioidentical progesterone using dutasteride (A 5α-reductase inhibitor): a pilot study. J Pharm Pharm Sci. 2010;13(4):626-36. doi: 10.18433/j3rw2h. PMID: 21486536.
5. Holzer G, Riegler E, Hönigsmann H, Farokhnia S, Schmidt JB. Effects and side-effects of 2% progesterone cream on the skin of peri- and postmenopausal women: results from a double-blind, vehicle-controlled, randomized study. Br J Dermatol. 2005 Sep;153(3):626-34.
6. Mircioiu, C., Perju, A., Griu, E. et al. Pharmacokinetics of progesterone in postmenopausal women. Eur. J. Drug Metab. Pharmacokinet. 23, 397–402 (1998). https://doi.org/10.1007/BF03192300
7. Kaestli LZ, Wasilewski-Rasca AF, Bonnabry P, Vogt-Ferrier N. Use of transdermal drug formulations in the elderly. Drugs Aging. 2008;25(4):269-80. doi: 10.2165/00002512-200825040-00001. PMID: 18361538.
8. Otberg N, Patzelt A, Rasulev U, et al. The role of hair follicles in the percutaneous absorption of topical progesterone. *J Invest Dermatol.* 1995;104(5):805–809. [PMID: 8054206]
(no abstract available)
 Environmental toxins have increased dramatically since the Second World War, and with them, the rise in hormone-related and degenerative diseases. Although all vertebrates are affected, these conditio…
Environmental toxins have increased dramatically since the Second World War, and with them, the rise in hormone-related and degenerative diseases. Although all vertebrates are affected, these conditio…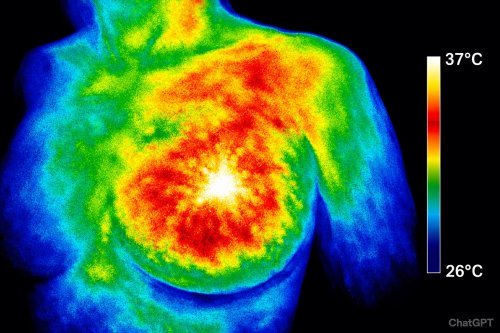
 Memory is the brain’s ability to store and recall information. When this system fails, we experience memory loss, which ranges from mild forgetfulness to severe cognitive impairment such as dementia o…
Memory is the brain’s ability to store and recall information. When this system fails, we experience memory loss, which ranges from mild forgetfulness to severe cognitive impairment such as dementia o… Migraines aren’t just intense headaches — they’re a systemic neurological crisis that disrupts your senses, drains your energy, and derails your life. What most people don’t realize is that women are…
Migraines aren’t just intense headaches — they’re a systemic neurological crisis that disrupts your senses, drains your energy, and derails your life. What most people don’t realize is that women are…