Inflammation
There are about 100 diseases that produce either inflammation in the connective tissues or degeneration of these tissues. These include...
- Alzheimer's
- Ankylosing Spondylitis
- Arthritis (osteoarthritis, rheumatoid arthritis, psoriatic arthritis)
- Asthma
- Atherosclerosis
- Crohn's disease
- Colitis
- Dermatitis
- Diverticulitis
- Hepatitis
- Irritable Bowel Syndrome (IBS)
- Lupus Erythematous
- Nephritis
- Parkinson's disease
- Ulcerative Colitis
Inflammation is the end result of long term oxidative stress. The stress can be caused by emotional or physical trauma, and nutritional or environmental pollutants. In most cases it is something of everything.
Interestingly the incidence of atherosclerosis, heart attack and stroke is greatly increased in rheumatoid arthritis (RA). All of which are due to oxidative stress.
The question is... 'what has caused the oxidative stress?'
Food is a major culprit, sugar being the number one culprit as it causes glycation. Sugar in any form, ie starchy carbohydrates like potatoes, legumes, sweet fruit or root vegetables, sugar in drinks, sauces, tinned food etc., and in particular grains and anything made from them such as bread, cakes, biscuits, pasta etc. These all convert to glucose.
Glycation occurs when a glucose molecule binds to a protein or lipid molecule without the control of an enzyme. This impairs the function of the molecule, leading to advanced glycation endproducts (AGEs), resulting in many of our inflammatory diseases.
Physical or mental stress also causes oxidation. Markers for inflammatory diseases are...
- low reduced glutathione (GSH) levels
- low vitamin D and other antioxidants
- high oxidised glutathione (GSSG) levels
- high malondialdehyde (a marker for oxidative stress, formed when fats are oxidised)
- increased lipid peroxidation
- high homocysteine
- high CRP
- high fructosamine
All these markers should be tested for.
Factors that cause inflammation...
- oxidative stress, due to decreased levels of antioxidants, in particular vitamin D, glutathione and superoxide dismutase. And an increase in sugar and foods which convert to glucose
- decreased zinc and selenium levels. Oestrogen suppresses zinc levels, progesterone raises them
- a deficiency of the essential fatty acid Omega 3
- decreased levels of vitamins B2, C, E and beta-carotene
- a high level of matrix metalloproteinases (MMP's), these enzymes break down protein causing a pathological reaction such as inflammation
- a high level of oestrogen. Oestrogen stimulates matrix metalloproteinases, it also accelerates the aging of collagen
- a lack of progesterone, this is always low in inflammatory diseases. Progesterone suppresses MMPs
- a predominance of the inflammatory Th1 cytokines over the anti-inflammatory Th2 cytokines. Progesterone stimulates the Th2 response, do does vitamin D
- emotional stress, progesterone calms by activating the GABA receptor sites, GABA is one of our most calming neurotransmitters
- allergies to certain foods. Oestrogen increases the response to allergens, progesterone suppresses mast cells responsible for the increase in histamine
- a high level of advanced glycation endproducts (AGEs)
- environmental pollutants
- a high level of tumor necrosis factor-alpha. Progesterone suppresses TNF-alpha
- a high level of prolactin. Progesterone suppresses prolactin, so does the amino acid tyrosine
- increased levels of fructosamine, a sign of insulin resistance
- increased levels of homocysteine
- increased copper levels. Copper suppresses both progesterone and zinc, supplementing with these two will suppress the excess copper
- a high level of pro-inflammatory HDLs, leading to increased lipid peroxidation. Progesterone protects against lipid peroxidation
About 1% of the world's population have rheumatoid arthritis. It's predominantly found in women, who have three times the likelihood of getting it than men. Although it can occur at any age, more often than not it occurs between the ages of 20 to 60.
In women it frequently begins during peri-menopause, i.e. between the ages of 40-50, with symptoms typical of oestrogen excess...
- general aches and stiffness
- pain in the joints
- fatigue and difficulty sleeping
Many find their symptoms increase just before menstruation when the progesterone level is low.
There is a predominance of the inflammatory Th1 cytokines over the anti-inflammatory Th2 cytokines in arthritis. Progesterone stimulates the Th2 cytokines, so pregnancy improves symptoms in 75% of cases. The reason for this is progesterone levels rise greatly during pregnancy, particularly in the third trimester, when symptoms in lupus patients abate.
It's tempting to speculate the remaining 25% do not get relief as their progesterone level was too low. An interesting corollary to this is that 90% of cases relapse within six months after giving birth, highest within the first three months. Progesterone levels fall sharply after birth.
But prolactin, the hormone governing milk production, rises after birth. Prolactin stimulates the immune response and is elevated in both male and female RA patients. Progesterone suppresses prolactin production.
Studies have found a progesterone deficiency in females with thyroid and ovarian autoimmune diseases. They have also found both progesterone and androgens were significantly lower during the luteal phase in RA patients. A rare case of systemic lupus erythematosus (SLE) occurred in a transgender man, who was given feminising hormones (oestrogen).
Natural treatment
Oxidative stress is evident, hence the inflammation, it's imperative this is reversed before long term damage occurs. High dose antioxidants should be taken, progesterone should be considered and foods containing sugar or converting to glucose should be avoided.
Progesterone is neuroprotective, it prevents lipid peroxidation and confers vascular protection. Both the endogenous steroid cortisol and the widely prescribed glucocorticoid prednisolone, increases cholesteryl ester (CE) formation, leading to atherosclerosis, progesterone blocks this increase. In contrast to progesterone, estradiol was ineffective.
As an anti-inflammatory agent, progesterone has been shown to reduce the response of natural killer cells, the Th1 cytokine response, as well as other known initiators of inflammation.
Progesterone suppresses oestrogen, which is an excitatory hormone, a known initiator of inflammation. Progesterone stimulates the production of IL-4 and IL-10, anti-inflammatory agents.
Progesterone increases levels of reduced glutathione and superoxide dismutase.
Matrix metalloproteinases (MMPs) are enzymes involved in the destruction of connective tissues in arthritis. Oestrogen maintains secretion of matrix metalloproteinases. In contrast, progesterone is a natural inhibitor of metalloproteinases.
Tumor necrosis factor-alpha is an inflammatory cytokine involved in the acute phase reaction in arthritis. Progesterone decreases both intracellular and secreted TNF-alpha, oestrogen has no effect.
Oxidative stress is behind all forms of inflammation due to low levels of antioxidants, these should be increased. In particular vitamin D and the amino acid N-acetyl cysteine.
Glutathione and vitamin D are our most important endogenous antioxidants.
Cysteine also chelates any excess copper and other environmental toxins. Selenium is an important addition, as it's part of the glutathione molecule. The other two amino acid precursors are glycine and glutamine, both these are usually found in abundance in food, cysteine is not. But if under stress, glutamine becomes a conditionally essential amino acid and supplementing is advisable.
If any emotional stress is being experienced, progesterone is excellent, as it activates the GABA receptor sites. This is an amino acid and also one of our most calming neurotransmitters. GABA itself is difficult to use, too much and symptoms return, it's far easier to use progesterone.
Taurine is another of our most calming neurotransmitters, a powerful sulphur amino acid like cysteine, it is also vital for the immune system, this should be considered too. It's vital for bile production, without it fats accumulate in the blood.
Insulin resistance should be checked for. If this is present it should be reversed, please see here.
If a high homocysteine level is found vitamins B2, B6, B12, folic acid, tri-methyl glycine and zinc should be taken.
Vitamin D is essential for health, have a blood test done to check the level. The test should only be done for 25-hydroxyvitamin D, also called calcidiol.
30-50% of people have a deficiency, particularly those living in climates with little sun, living above 32 degrees north or south of the equator, work in doors and spend little time in the sun.
Levels should be between 50-100ng/mL or 124.80-249.60nmol/L. A deficiency is less than 25ng/L or 62.4nmol/L. For more information please see here.
Additional information
Progesterone
The amount to use will be dependant on the individual and the severity of the problem. Women should use between 100-200mg of progesterone daily, men should use between 10-100mg/day. In severe cases more might be needed. Vary the amount used following symptoms as a guide. Rubbing progesterone cream directly onto arthritis affected joints has helped many sufferers.
For more information on how to use progesterone please see here.
Before using progesterone it's essential to read the page on oestrogen dominance first.
The following plants contain powerful antioxidants...
- green tea (catechins)
- raspberries, strawberries, blackberries, cranberries, walnuts, and pecans all contain ellagic acid, the greatest amount is found in raspberries
- glucosinolates, potent inducers of Phase II enzymes, found in the brassica family, i.e. broccoli, cabbage, watercress etc., avoid eating too many of these raw as they are goitrogens, they contain an enzyme that suppresses the thyroid gland. Alternatively take 200mg indole 3 carbinol, an extract from the brassicas
- The spice turmeric contains curcumin, which has been found to stop pre-cancerous changes in the DNA
- many plants contain flavonoids, particularly berries and buckwheat, which remove metal toxins and also protect the antioxidant vitamins.
Please see here for more information on Nutrition and Diet.
Tests for inflammation
1. Vitamin D (low) (essential test). The test should be done for 25-hydroxyvitamin D, also called calcidiol. The following list gives an indication of levels of vitamin D found in the blood (ZRT Lab):
- Sufficient 50-100ng/ml or 124.80-249.60nmol/L
- Hypovitaminosis less than 30ng/ml or 75 nmol/L
- Deficiency less than 25ng/ml or 62.4nmol/L
2. CRP (increased levels) (essential test). The level of CRP rises when there is inflammation throughout the body, normally none should be found. Levels if found, vary from <1.0mg/L to >3.0mg/L (Medline CRP).
3. Homocysteine (possibly increased levels) 0.54-2.3 mg/L (4-17 micromoles per liter (mcmol/L). WebMD
4. Malondialdehyde (increased)
Standard Range: 1.0 - 4.0 mM
Northwest Life Science Specialties
Baylor Research Institute
5. Progesterone (generally low) (Medline Progesterone)
- Serum 10 ng/ml
- Saliva 0.2 ng/ml
6. Oestradiol (possibly high) (Medline Oestradiol)
- Serum 30 to 400 pg/mL
- Saliva 2 pg/ml
7. Insulin resistance (sometimes observed). There is no single test for IR, but the following are often tested (Medline Insulin resistance) (Lab Tests Online - Understanding insulin resistance)...
- Blood pressure equal to or higher than 130/85 mmHg
- Fasting blood sugar (glucose) equal to or higher than 100 mg/dL
- Elevated insulin levels
- Elevated CRP (a marker for inflammation)
- Large waist circumference - 35 inches (87.5cm) or more
- Low HDL cholesterol - Under 50 mg/dL
- Triglycerides equal to or higher than 150 mg/dL
Online references
Adverse side effects...
 If you are feeling confused or overwhelmed by fertility challenges, or wondering if hormone balance might be affecting your ability to conceive you are not alone—many women and couples face uncertaint…
If you are feeling confused or overwhelmed by fertility challenges, or wondering if hormone balance might be affecting your ability to conceive you are not alone—many women and couples face uncertaint…
 _____
_____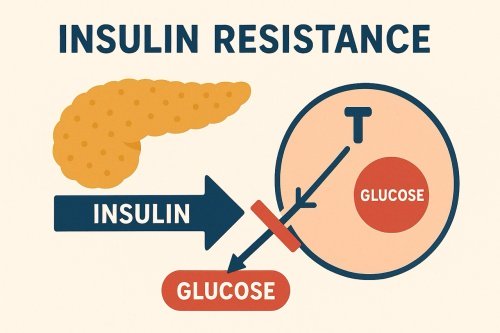 Feeling tired, foggy, or struggling with stubborn weight gain—especially around the waist? You might be surprised to learn that these symptoms could be linked to insulin resistance, a condition that a…
Feeling tired, foggy, or struggling with stubborn weight gain—especially around the waist? You might be surprised to learn that these symptoms could be linked to insulin resistance, a condition that a…